Description 1,2,3,4
Plantar fasciitis is a common foot disorder that results in heel pain on weight bearing. The pain occurs at the origin of the plantar aponeurosis, at the anteromedial aspect of the calcaneus. This condition is typically self-limiting and can most often be managed with conservative treatment but may take up to 12-18 months to resolve completely. In rare, but more severe cases, surgery may be needed.
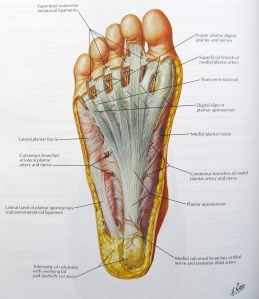
Anatomy 2-6
The plantar aponeurosia/fascia is a thick band of fascia that covers the structures on the bottom of the foot. It runs from the medial tuberosity of the calcaneus and broadly extends the length of the foot and divides into five bands. Each band attaches onto the base of the proximal phalanx of each toe. The fascia can be divided into three components, medial, lateral, and central. The central component is associated with plantar fasciitis. The fascia also acts as a shock absorber during gait and is the main support of the longitudinal arch of the foot.
The plantar fascia and associated structures of the foot have been identified as the Windlass Mechanism. The calcaneus, midtarsal joint, and metatarsals form the truss’s arch, while the plantar fascia forms the tie-rod. When the foot is dorsiflexed during the propulsive phase of gait, the plantar fascia winds around the head of the metatarsals, drawing the calcaneus closer and elevating the arch.
Incidence/Prevalence 1-5
Plantar fasciitis is the most common cause of heel pain, occurring in over 10 percent of the population. It most frequently presents in individuals,typically women, between the ages 40-60 years old and people who weight bear for extended periods of time such as athletes and occupations that require prolonged standing. Improper footwear and abnormal foot biomechanics, particularly over-pronation can all put increased tension placed on the soft tissue in the plantar aspect of the foot, increasing the potential risk of developing plantar fasciitis.
Clinical Presentation 2-4
The diagnosis of plantar fasciitis is based on the patient’s history and clinical examination. Patients present most commonly with:
- Pain and tenderness localized on the medial aspect of the heel
- Pain that increases with the first steps in the morning or with walking after long durations of non-weight bearing.
- Pain lessens with activity
- Pain is most often unilateral
Potential Etiologies 2,4,7
The etiology of plantar fasciitis is still unknown. When the condition was given the title plantar fasciitis, fasciitis meaning inflammation, that was thought to be the cause. However, histologic studies have actually refuted this theory and found it to be due more to degeneration and repetitive microtrauma at the origin of the fascia. Over time these microtears, due to increased stress on the fascia, result in a macro injury causing pain in the heel. This can be caused by increase physical activity or increased durations of being on your feet.
Diagnostic Tests 2,4,8
Diagnostic tests are usually utilized in order to rule out other causes of heel pain and if previous treatment has failed. They are not particularly helpful in identifying plantar fasciitis. Heel spurs are commonly found using radiography in patients with plantar fasciitis but has not been proven to be a cause.
Evaluation 2,4
In an evaluation for plantar fasciitis, the foot and ankle should be analyzed during both stance and gait, pes planus or pes cavus can increase loading. Achilles tendon contracture is often coupled with plantar fasciitis because the foot is plantarflexed causing the heel to come off the ground earlier in the stance phase of gait, stressing the plantar fascia. Evaluating the spine and lower extremities can identify any neurologic component to symptoms. Location of the pain is the most important factor of the evaluation and will provide the most information.
Conservative Treatment
Plantar fasciitis is a self-limiting condition and conservative treatment works for over 80% of patients but may take up to 12-18 months to complete resolve. The main focus of treatment is to stretch the fascia and reduce the stress applied to it. Stretching techniques and foot orthotics are typically the first approaches to treatment and usually the most effective. The following are used in combination or in a second attempt if previous treatment has failed. 4
- Stretching- Most protocols emphasize stretching the Achille’s tendon, however a non-weight bearing stretch specific to the plantar fasciitis has been shown to be like most effective in regards of reducing pain and improving function. The stretch is performed by resting your foot over the opposite leg, then grabbing the toes and pulling them towards the shin. A stretch should be felt in the arch. Hold the stretch for 15-20 seconds and repeat several times a day, most importantly before you get out of bed in the morning. 2,9,10
- Orthotics- prevents abnormal motion of the foot and reduces over pronation by supporting the medial arch. Most commonly used orthoses are prefabricated silicone/rubber heel cups, prefabricated arch supports, felt pads, and custom arch supports. The following video is a demonstration of how heel cups can reduce and treat pain. 1,2,4
- Ice- Massaging foot over a frozen water bottle will relieve pain, massage and stretch the plantar fascia
- Massage 3,4
- Weight loss 1,5
- Extracorporeal Shock Wave Therapy- There is inconsistant evidence as to whether this is truly effective in the treatment of plantar fasciitis. It has been shown to possibly be effective in treating runners with chronic symptoms. 2,4,11
- Injections 8
- Night splints- keep the plantar fascia and the calf stretched out during sleep when normally the foot rests in a plantar flexed position which is in the shortened position and will tighten the plantar fascia. However, evidence does not strongly support its effectiveness. 2,4
- Taping- the effectiveness of taping techniques are still unknown. The following video demonstrates a technique used on athletes. 8
Physical Therapy Management of Plantar Fasciitis
Surgery and Post-op Treatment 2,4,10
For the small percent of patients that do not see results from conservative treatment, typically symptoms persisting over a year, surgery may be an option. However, most surgical methods do not have an encouraging outcome and often do not result in full function. It is ideal to consider all conservative treatment options first before electing the surgical route.
Additional Resources
http://www.aafp.org/afp/2005/1201/p2237.html#afp20051201p2237-b17
References
- Stuber K, Kristmanson K. Conservative therapy for plantar fasciitis: a narrative review of randomized controlled trials. J Can Chirop Assoc. 2006;50(2):118-133.
- Neufeld SK, Cerrato R. Plantar fasciitis: evaluation and treatment. J Am Acad Orthop Surg. 2008;16(6):338-346.
- Wearing SC, Smeathers JE, Urry SR, Hennig EM, Hills AP. The pathomechanics of plantar fasciitis. Sports Med. 2006;36(7):585-611.
- Jariwala A, Bruce D, Jain A. A guide to the recognition and treatment of plantar fasciitis. Primary Health Care. 2011;21(7):22-24.
- Natali AN, Pavan PG, Stecco C. A constitutive model for the mechanical characterization of the plantar fascia. Connective Tissue Research. 2010;51:337-346.
- Bolgla LA, Malone TR. Plantar fasciitis and the windlass mechanism: a biomechanical link to clinical practice. J Athl Train. 2004;39(1):77-82.
- Barrett SL, Erredge SE. Growth factors for chronic plantar fasciitis? Podiatry Today. http://www.podiatrytoday.com/article/3151. Published 2004. Accessed November 28, 2011.
- Cole C, Seto C, Gazewood J. Plantar fasciitis: evidence-based review of diagnosis and therapy. Am Fam Physician. 2005;72(11):2237-2242.
- DiGiovanni BF, Nawoczenski DA, Lintal ME, Moore EA, Murray JC, Wilding GE, Baumhauer JF. Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain. A prospective, randomized study. J Bone Joint Surg Am. 2003;85-A(7):1270-1277.
- DiGiovanni BF, Nawoczenski DA, Malay DP, Graci PA, Williams TT, Wilding GE, Baumhauer JF. Plantar fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis. J Bone Joint Surg Am. 2006;88-A(8):1775-1781.










