Summary of the Condition
A total shoulder replacement (TSR) is when the articulating surfaces that make up the glenohumeral shoulder joint are replaced. The humeral head and the glenoid fossa are removed and replaced with artificial implants to create a smoother gliding surface. During the surgery the anterior deltoid and anterior capsule are cut and the subscapularis tendon distal attachment is removed in order to get to the joint surfaces. So, these structures must not be over stressed during rehabilitation. A TSR is done as an intervention due to a patient’s co-morbidity with the goal to decrease chronic shoulder pain and improve a patient’s functional mobility.

[http://www.vejthani.com/web-english/Total-shoulder-replacement.php]
Guide to PT Practice: Practice Pattern and Suggested Management
Link to Guide of Physical Therapy
The Guide to PT Practice gives 4H: Impaired Joint Mobility, Motor Function, Muscle Performance, and Range of Motion Associated With Joint Arthroplasty, for a total shoulder replacement. The guide recommends 12-60 treatment visits.
The electrotherapeutic modalities that the guide finds appropriate for this population are biofeedback and electrical stimulation. The electrical stimulation types includes: electrical muscle stimulation (EMS), functional electrical stimulation (FES), high voltage pulsed current (HVPC), neuromuscular electrical stimulation (NMES), transcutaneous electrical nerve stimulation (TENS).
The physical agents within a 4H diagnosis include: cryotherapy, hydrotherapy, ultrasound, phonophoresis, and thermotherapy. The continuous passive motion (CPM) is listed as a mechanical agent available for this practice pattern, however, not commonly seen with TSR.
Relieving Pain and Swelling
There are no specific research studies identifying the modalities that are affective with postoperative TSR. However, there are many protocols/guidelines that advise using:
- Cryotherapy: 20min x 3/day 1 and after exercise2
- Anti-inflammatories 2
- Sling: 3-4 weeks postoperative3
- Other modalities are not specified for a TSR rehab, but one protocol advises to use of pain relieving modalities as needed. 1
Increasing Strength and ROM
There is little research done on effective strengthening programs after a TSR. However, there is heavy emphasis on the important role rehabilitation has in gaining maximal functional performance and decrease in patient’s pain. Each patient’s rehabilitation is primarily directed by their underlying pathology that is caused the need of a TSR. 4
The physical therapy rehabilitation protocol below draws heavily from the following protocol Brigham and Women’s Hospital, created by Reg. B Wilcox III.3 Rehabilitation progresses through four phases. Each phase has criteria to progress to the next phase as well as a time frame standard in order to allow enough soft tissue healing to occur.3 There are additional exercises added to the protocol. Please refer to link for the specific protocol used by Brigham and Women's Hospital.
PHASE I: Post-operative day 1 – 4 weeks
- ROM
- Passive ROM only
- Forward flexion in supine to tolerance
- Gentle ER in scapular plane to available PROM usually around 30º
- IR to chest
- Pendulum
- A small study showed that doing pendulums with or without a weight does not have an effect of muscle relaxation (measured with EMG) during the exercise. Subjects that did have a shoulder pathology did have a more difficult time relaxing their supraspinatus and upper trapezius.5
- Passive ROM only
[http://www.youtube.com/watch?v=gn4LDOkWRHk]
- Strengthening
- Active distal extremity exercises: elbow, wrist, hand
- AROM progressing to strengthening exercises as appropriate
- Scapula: retraction and elevation AROM and isometric exercises

[http://athleticsandaesthetics.wordpress.com/2011/09/15/the-finer-points-of-overhead-squatting/]
Exercises in the beginning should be low number of repetitions and for short, frequent sessions.2 As patient progresses, begin assisted flexion, ER, and IR in the scapular plane. Progress distal extremity exercises as appropriate for patient.
In order to progress patient to the next phase, the patient must reach the criteria below:
- Tolerates PROM program
- At least 90º PROM forward flexion and elevation in the scapular plane
- At least 45º PROM ER in the scapular plane
- At least 70º PROM IR in the scapular plane measured at 30º of abduction
If patient has not reached this, then continued gradual ROM and gentle mobilization of grade I oscillations is necessary. Soft tissue restraints should always be considered with ROM exercises.
PHASE II: Early strengthening - 4-6 weeks after surgery

- ROM
- Continue PROM and AAROM
- Within pain free range: begin active flexion, IR, ER, elevation in the scapular plane
- Wand exercises in each direction allowing affected arm to take more weight through motion2
- Arm-sliding on the table2
- AAROM pulleys: >90º PROM
- Begin horizontal AAROM
- With wand or manually2
- Gentle glenohumeral and scapulothoracic joint mobilizations as indicated
- Grade I, possibly Grade II
- Initiate glenohumeral and scapulothoracic rhythmic stabilization
[http://ukhcforums.uky.edu/cartilage/postop_care/shoulder_exercises.htm ]
- Strengthening
- Continue appropriate scapular strengthening and progress accordingly: isometrics and manual scapular resistance
- Body Blade 1
- One-handed grip in neutral position
- Two-handed grip in front
- Opposite hand diagonal patter
- Body Blade 1
- Progress distal joint strengthening with light resistance
- Continue appropriate scapular strengthening and progress accordingly: isometrics and manual scapular resistance
[http://www.government-medical-supply.com/bodyblade-bodybladepro.html]
Criteria to progress to the next phase:
- Tolerates P/AAROM, isometric program
- At least 140º PROM forward flexion and elevation in the scapular plane
- At least 60+º PROM ER in the scapular plane
- At least 70º PROM IR in the scapular plane measured at 30º abduction
- Able to actively elevate shoulder against gravity with good mechanics to 100º
Again, if patient is not able to complete the ROM indicated above continue gradual ROM and mobilizations, Grade I oscillations, to progress patient.
PHASE III: Moderate strengthening
This phase should not start prior to the 6 week mark in order to allow for proper soft tissue healing to occur.
- ROM
- Progress AROM exercises as appropriate
- Advance PROM to stretching as appropriate
- Continue PROM in order to maintain ROM
- Start assisted IR behind back stretch
- Progress from AAROM to AROM avoiding large stress to the anterior capsule

[http://breastcancer.about.com/od/lifeaftertreatment/ss/arm_exercises_tutorial_9.htm]
- Strengthening
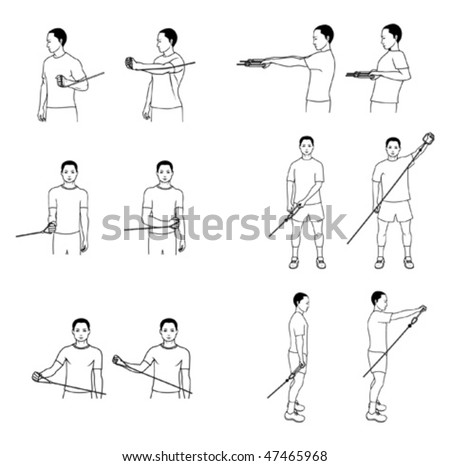
- Resisted shoulder IR, ER in scapular plane
- Manual resistance or holding a light weight or using a light resistance theraband
- Begin progressive supine active flexion strengthening (anterior deltoid)at varying ranges with light weights
- Progress with light resistance theraband in the scapular plane
- Resisted shoulder IR, ER in scapular plane
Criteria in order to move on to the next phase:
- Tolerates AA/AROM/strengthening
- At least 140º AROM forward flexion in scapular plane supine
- At least 60+º AROM ER in scapular plane
- At least 70º AROM IR in scapular plane supine with 30º of abduction
- Elevate shoulder standing with proper mechanics to at least 120º
- * if patient is meeting the ROM standard within their underlying pathology then the patient is ready to progress
PHASE IV: Advanced strengthening
Do not begin prior to the 12th week in order for appropriate soft tissue healing, ensure adequate ROM has been achieved, and initial strengthening program has had time to take affect.
- Strengthening
- Progress strengthening program
- Avoid putting stress on the anterior capsule and surrounding structures
- Progress strengthening program
Functional Activities
Begin functional activities at phase III but, no earlier than week 6. Then gradually progress intensity through week 12. Patient can expect return to recreational activities 4-6 months if no complications interfere with the patient’s rehab.3
For example, if progressing a patient to playing a full round of golf, you can start with wand ROM with swing within available, pain free range. Then progress with putting then easing into a full swing.

[http://www.clipartof.com/gallery/clipart/golfing_2.html]
Home Exercise/Modality Use
Patients are advised to ice 20 min 3 times a day and then as needed after exercise and for pain management.1
Majority of the ROM and strengthening exercises can be done at home if patient can demonstrate knowledge of proper techniques and precautions. Each underlying pathology will fluctuate each patient’s progress, timeline, and expectation/goals from physical therapy. A home exercise program will differ from each patient.
Special Instructions
- Sling should be worn 3-4 weeks after surgery unless otherwise instructed by surgeon. Then progressively decrease sling use over the next 2 weeks
- During 6-8 weeks a small pillow should support elbow while lying supine.
- No driving for 3 weeks.
- No lifting objects till week 4-6, then no lifting heavier than a coffee cup till week 6-12.
- No jerking or pushing motions.
- Do not allow shoulder to support body weight through the arm till week 8.
- Each surgeon will have specific precautions they want their patients to follow.
TSR Protocols
Case Western Reserve University; Reuben Gobezie, M.D
Beth Israel Deaconess Medical Center
Brigham and Women's Hospital










