Osgood Schlatter's Disease
General Description
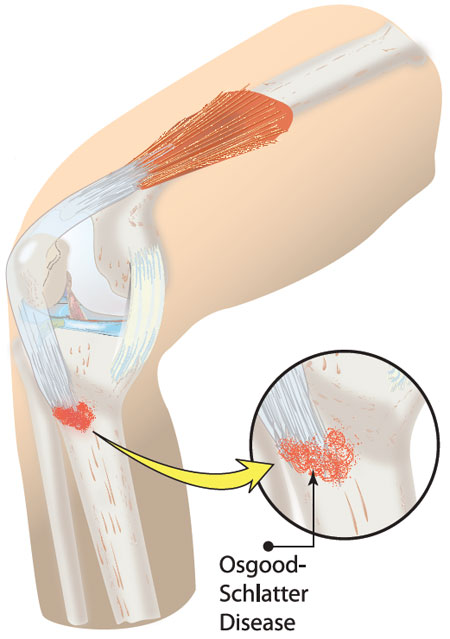
The term Osgood Schlatter's Disease was coined by an American orthopedist, Robert B. Osgood, and a Swiss surgeon, Carl Schlatter.1 This condition is most common in children that actively participate in sports that require running and jumping activities. These include, but aren't limited to, basekball, soccer, track, cross country, soccer, ballet, and gymnastics.2 Osgood Schlatter's is described as an osteochondritis or apophysitis on the patellar tendon attachment to the tibial tubercle.1,3 In general, osteochondritis is an inflammation of a bone and its associated cartilage. Apophysitis is inflammation of a bony outgrowth that is still attached to the bone. In the case of Osgood Schlatter's Disease this bony outgrowth is the tibial turberosity that is still attached to the bone in the lower leg known as the tibia. This condition is characterized by anterior knee pain. Conservative treatment is successful in many cases; however, surgical intervention does exist for this condition.4
Anatomy
When discussing the anatomy associated with Osgood Schlatter's Disease, it is important to understand the anatomy of the anterior knee as it relates to this condition.
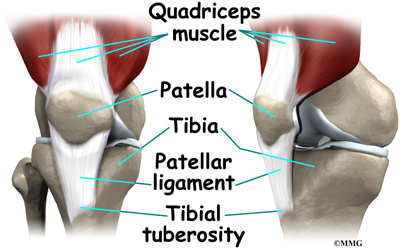
Referring to the picture to the left, you see the quadriceps muscle. This muscle is located in the thigh on both the right and left sides of the lower extremity. This muscle is composed of four muscles: the rectus femoris, vastus lateralis, vastus medialis, and the vastus intermedius. The rectus femoris muscle originates on the anterior superior iliac spine. When it concentrically contracts (shortens) it causes flexion at the hip along with extension at the knee. The remaining three quadriceps muscles originate on the femur and function to extend the knee. The four quadriceps muscles come together to form the common quadriceps tendon (also referred to as the patellar tendon) that inserts into the superior (upper) aspect of the patella. The patella is a sesmoid bone. A sesmoid bone is bone that is embedded in a tendon that creates a mechanical advantage for the action of the muscle that attaches to that tendon. At the inferior (lower) aspect of the patella, the patellar ligament (also referred to as the patellar tendon) begins and inserts into the tibial tuberosity of the tibia (also referred to as the shin bone). The insertion of the patellar ligament into the tibial tuberosity is the location of the injury associated with Osgood Schlatter's Disease.
Image Source: http://www.concordortho.com/patient-education/topic-detail-popup.aspx?topicID=9c2c5ae2333ff1b24f5fb4a3abba8184
Etiology
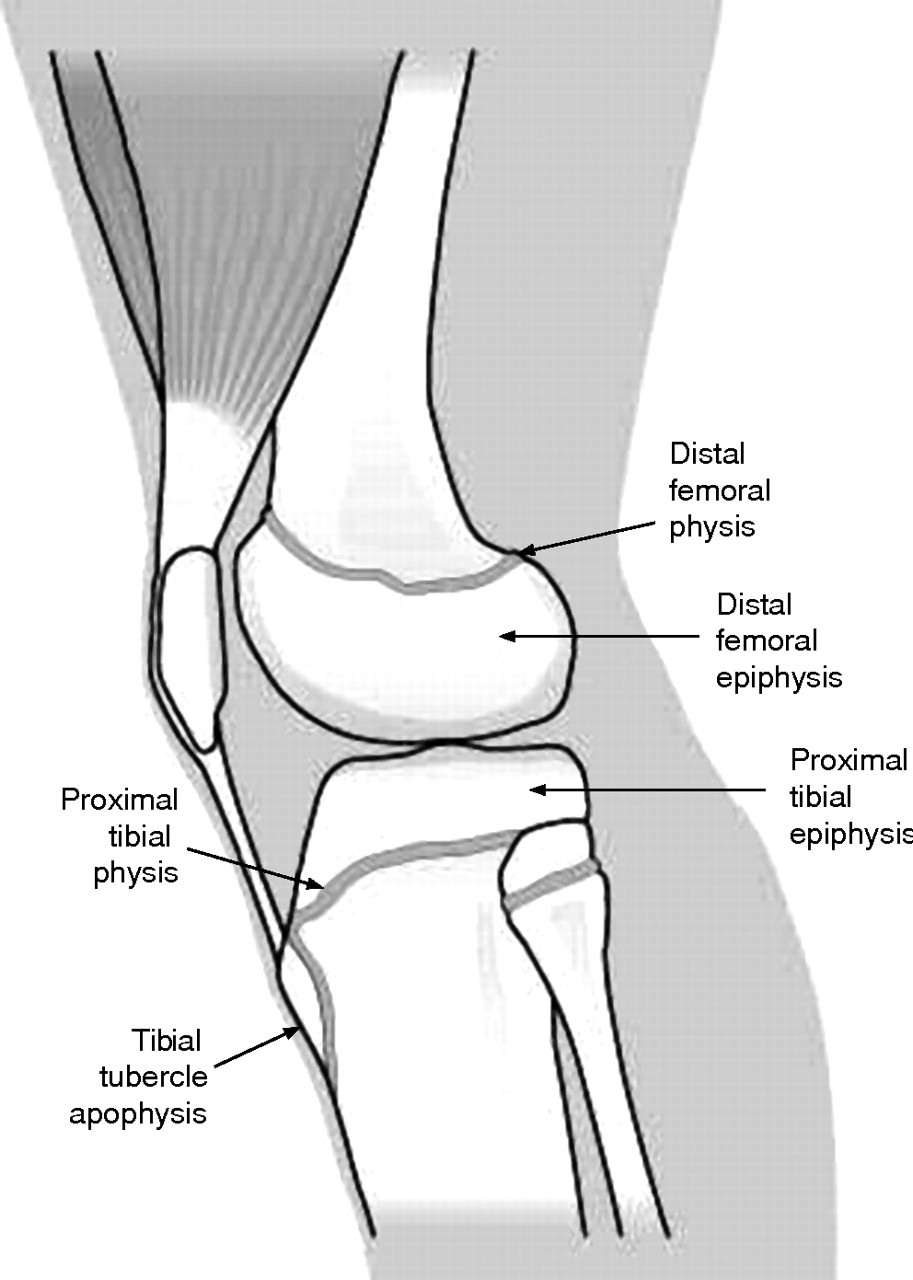
Epiphyseal plates are located in the long bones of prepubescent adolescents. There are four stages involved in the elongation of this bone. There is a cartilaginous stage that occurs between the ages of 0 - 11 years. The following stage occurs between the ages of 11 - 14 years of age and is called the apopyseal stage. The most cases of Osgood-Schlatter occur during this stage. Between the ages of 14 - 18, the bone is in the epiphyseal stage. By the age of 18, the bone has reached the bony stage in which the epiphysis is fused.5 The epiphyseal plate is where lengthening of the bone occurs during bone growth, and it is made up of cartilage.2 Cartilage isn't as strong as bone.3 The growth plate near the tibial tuberosity has three zones that grow and gradually merge together. The proximal zone is the same as the growth plate located on the superior aspect of the tibia. This is formed of short cell columns. The middle zone is composed of a substance with a high tensile strength called fibrocartilage, and it is covered with layers of hyaline cartilage. Fibrous tissue is the main component of the distal end.5 You can see the location of the epiphyseal plates on the tibia in the image to the right. Repeated contraction in the quadriceps muscle due to running, jumping, squatting, and other sports activities during the preossification phase causes repeated pulling on the tibial tuberosity by the patellar ligament.4 Due to the repetitive contraction, there is repeated avulsion of the patellar ligament at the apophysis of the tibial tubercle.3 An avulsion occurs when the pull of the patellar tendon due to quadriceps contraction causes the tibial tuberosity to pull away from the tibia creating an avulsion fracture. Pain is generated due to this avulsion. If continued contraction of the quadriceps in activity continues, the process of inflammation associated with bone injury is re-initiated. An increase in tension on the tibial tuberosity during quadriceps contraction may occur in adolescents with patella alta (the patella is higher in the patellar groove), patella baja (the patella is low in the patellar groove), genu valgum, internal rotation, and a more proximal and border insertion into the tibial tuberosity above the tibial physis.5 These conditions cause lengthening, shortening, or a change in orientation of the patellar tendon. These changes can cause an alteration of the vector of force generated on the tibial tuberosity during contraction of the quadriceps.5 Once rest occurs or the epiphyseal plate closes, the bone is able to heal itself by osteoblastic activity.1 A cartilaginous fragment exists initially when the trauma is occurring. After rest, the octeoblasts place new bone cells in the area creating a bony callus. Over time with weight bearing, this bone callus hardens into cortical bone. This creates an enlargement of the tibial tuberosity.3
Image Source: http://bjsm.bmj.com/content/40/9/749.full
Incidence and Prevalence
Osgood Schlatter's Disease affects about 1 in 5 adolescent athletes.2 Originally this condition was believed to be more prevalent in males than females. However, because more girls are participating in sport every year, this gender gap is becoming more equalized.2 The condition is seen in males between the ages of 12 and 15 years old. The age range that it is commonly see in females is 8 to 12 years old due to the earlier onset of puberty and associated epiphyseal plate closure in females.5 The condition itself is more common in patients that experience a rapid growth during adolescence that is higher than adolescents of their age.6 Osgood-Schlatter's Disease most commonly occurs bilaterally; however, it can only be localized to one side.5
Clinical Presentations
Patients with Osgood Schlatter's Disease typically initially complain of pain in the anterior knee after sporting activity.5
Other signs and symptoms include:
- Gradual onset of pain with no specific mechanism of injury5
- Tightness in the quadriceps muscle2
- Tightness in the hamstring muscles2
- Tightness in the gastrocnemius(bibcite 2))
- Swelling and inflammation of the knee3
- Point tenderness over the area of the tibial tuberosity3
Image Source: http://www.betterbraces.com/injury-info-center/knee-injury-guide/osgood-schlatter-disease
Pain in the anterior knee can be severe and continuous in the acute phase.((bibcite 5) A physician or emergency room should be consulted if the pain interferes with the individual's ability to complete activities of daily living due to pain, is associated with swelling or redness about the joint, and is associated with a fever. This can indicate an infection that may need medical treatment.2
Diagnostic Testing

Magnetic Resonance Imagining (MRI) is often done to rule out fracture or any other serious pathology. The MRI is taken from a lateral view with the leg internally rotated 10 - 20 degrees. MRI imaging may show normal, early, progressive, terminal, and healing stages of this condition.5 If the MRI is normal, the individual may just be in really early stages of Osgood Schlatter's Disease. A normal MRI should not be the only reason for ruling out this diagnosis. If there are symptoms, management may be necessary to help prevent the progression. Early and progressive stages may show anterior soft tissue swelling as well as the beginning of the separation between the tibial tuberosity and the tibia.5 The terminal and healing process stages show ossification and enlargement of the tibial tuberosity.7 A bony ossicle may still be visible on imaging even after fusion of the tibial epiphysis.5 The MRI image below shows avulsion of the tibial tuberosity from the tibia that is commonly seen in early and progressive stages on the condition. X-ray of the area can reveal the pulling away of the tibial tuberosity from the bone as well as any fractures that may be present.
Image Source: http://ookaboo.com/o/pictures/topic/12850704/OsgoodSchlatter_disease
Evaluation/Special Testing
Evaluation and diagnosis of Osgood Schlatter's Disease is often clinical. There is an association between age, sports activity, and symptoms that often leads the clinician to this diagnosis. Observation and palpation of the knee may reveal the characteristic enlarged mass over the tibial tuberosity. The image below shows the appearance of a knee without Osgood Schlatter's in comparison to someone in the healing stage of Osgood Schlatter's Disease.5 The individual on the left side does not have Osgood Schlatter's disease while the individual on the right has bilateral Osgood Schlatter's disease noted by the large tibial tuberosity.

Image Source: http://theringwoodclinic.blogspot.com/2011/08/knee-pain-in-children-10-16yrs-osgood.html
A second aspect of the evaluation is pain over the tibial tuberosity during resisted knee extension. The video below shows one example of how this is performed.
Conservative Treatment
Physical Therapy Management of Osgood Schlatter's Disease
Conservative (or non surgical) treatment for Osgood Schlatter's Disease is a team approach that should involve a physical therapist, a physician, the athlete, the guardian of the athlete, and the athlete's coach if necessary. In general treatment consists of ice, limitation of physical activity, oral inflammatory medications, protective knee padding/taping, and physical therapy for stretching and strengthening.5 Limitation of physical activity, physical load restriction, and conservative treatment has been shown to be more effective in research by Gerulis et al8 than physical load restriction alone. Patients with conservative treatment in combination with a participation restriction displayed a faster return to asymptomatic sport than patients without conservative treatment.
Conservative treatment done with a physical therapist should focus on stretching and low-intensity quadriceps strengthening exercises. Stretching exercises should include the musculature surrounding the knee: the quadriceps, hamstrings, iliotibial band, and gastrocnemius. Low-intensity strengthening of the quadriceps exercise should occur after an appropriate rest period of approximately 6 - 8 weeks. High-intensity exercise is introduced gradually as the quadriceps strengthens and pain decreases. Introduction of these high-intensity exercises to soon can result in a recreation of the pain.5 Below is a graphic representation of some of these exercises. A physical therapist should be consulted before starting an exercise program to ensure the exercises are being done correctly.
Injection of a solution of 1% lidocaine with a 12.5% dextrose has been investigated for treatment of Osgood Schlatter's Disease. Results of a study by Topol et al9 show that return to sport with no symptoms occurred more frequently in patients treated with the lidocaine and dextrose injections than patients treated with just lidocaine injection or usual treatment. These researchers also indicated that in their study population asymptomatic sport participation was more common in the patients injected with the lidocaine and dextrose at a one year followup than patients injected with just lidocaine or the usual treatment.9
Taping techniques that put compression on the patellar ligament are used, but these taping techniques have not been determined to be effective by scientific research. The following video shows a kinesiotape technique for Osgood Schlatter's Disease.
Surgical Treatment
Surgical treatment of Osgood Schlatter's Disease involves a skin incision, shaving of the tibial tuberosity, removal of any bone spurs, and bone plugs to reposition the tibial tuberosity. Specifically, there is drilling of the tibial tubercle, excision of the tibial tubercle, excision of the ununited ossicle and free pieces of cartilage, insertion of bone pegs to reattach the tibial tubersity, or a combination of all of these procedures.5 El-Husseini et al10performed a study on adults with unresolved Osgood Schlatter's Disease. The procedure performed involved tibial tuberosity reduction osteotomy. The researchers reported a reduction in pain with an increased ability to kneel without pain in the adults that had undergone surgery.10 Adolescent individuals do not typically need surgical intervention. If conservative treatment and rest are performed, adolescents typically heal resulting in no need of surgical intervention.
Prognosis
Prognosis for individuals with Osgood Schlatter's Disease is good. Most individuals (90%) have spontaneous resolution of the condition once the epiphyseal plates have ossified (around 18 years old). Before this time, symptoms can be self-limiting; however, with proper conservative management no limitation should be present. The remaining 10% of patients have symptoms that continue into adulthood regardless of conservative treatment.
It is important to note that studies have been done on college athletes with a history of Osgood Schlatter's Disease in comparison to collegiate athletes without a history of Osgood Schlatter's disease. Using the Knee Outcome Survey Activities of Daily Living and Sport Activity Scale as outcomes, the study indicated that individuals with prior history of Osgood Schlatter's Disease experienced higher levels of disability.10 This is why early recognition, rest, and conservative treatment are necessary.
Prevention
There are no prevention strategies that have been proven in scientific research to work. Clinicians suggest adolescent athletes participating in regular strengthening, stretching, and conditioning programs. Proper warm up and cool down after athletic activity are also beneficial to adolescent athletes.
Differential Diagnosis
Sinding-Larsen-Johansson Syndrome: Children present with SLJS around the same time period as Osgood Schlatter's Disease. This is generally around the ages of 10 to 12 years old. The patient complains of pain on the inferior patella with SLJS rather than over the tibial tuberosity which is characteristic of Osgood Schlatter's Disease.5 It is caused by repeated strain on the inferior aspect of the patella where the patellar ligament originates. In the later stages, x-ray may show degeneration.3
Image Source: http://freeimagefinder.com/user/33772445@N07.html
Hoffa's Syndrome: The infrapatellar fat pad has high nerve innervation. When there in impingement or inflammation of this structure, there will be excessive pain. The pain is located over the anterior knee. Tenderness is noted the most in the anterior joint line lateral to the patellar ligament. X-rays are typically normal while MRI usually reveals a low signal in the fat pad.5
Image Source: http://www.aidmyachilles.com/tendon-muscle-injuries-in-the-leg/hoffas-syndrome.php
Other differential diagnosis that must be evaluated include synovial plica injury, tibial tubercle fracture, infection, or tumor.5













