Muscles and Ligaments

Image Source
Wrist Flexors:Flexor Carpi Radialis, Flexor Carpi Ulnaris, Palmaris Longus, Flexor Digitorum Profundus/Superficialis,
Wrist Extensors: Extensor Carpi Radialis Longus, Extensor Carpi Radialis Brevis, and Extensor Carpi Ulnaris
Finger MP Flexion: Lumbricales and Interossei
Finger PIP and DIP Flexion: Flexor Digitorum Superficialis and Flexor digitorum profundus
Finger MP Extension: Extensor Digitorum, Extensor Indicis, and Extensor Digiti minimi
Finger Abduction: Dorsal Interossei
Finger Adduction: Palmer Interossei
Thumb MP and IP Flexion: Flexor Pollicis Bravis and Flexor Pollicis Longus
Thumb MP and IP Extension: Extensor Pollicis Bravis and Extensor Pollicis Longus
Thumb MP and IP Abduction: Abductor Pollicis Bravis and Abductor Pollicis Longus
Thumb adduction: Adductor Pollicis
Thumb to little finger Opposition: Opponens pollicis and Opponens digiti minimi
Blood Supply to the Hand
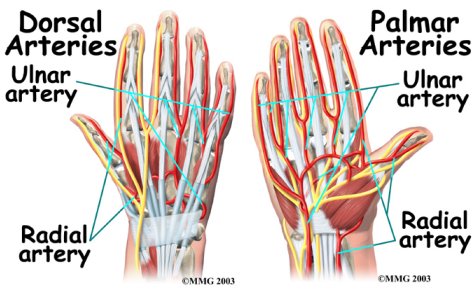 Image Source Image Source |
 Image Source Image Source |
Nerves of the Hand
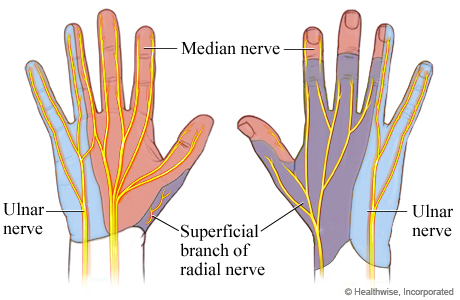 Image Source
Image Source
Intrinsic Muscles
The intrinsic muscles of the hand are the muscles that originate and insert in the hand itself. They are responsible for the movements of the the digits and position grip.
Lumbricals
The Lumbricals flex the metacarpalphalangeal joints and extend the interphalangeal joints of digits 2-5. Lumbricals 1-2 are innervated by the median nerve whereas lumbricals 3-4 are supplied by the deep branch of the ulnar nerve. The lumbricals attach to the tendons of flexor digitorum profundus and insert on the extensor hood. Lumbricals 1-2 are unipennate and lumbricals 3-4 are bipennate.
 Image Source
Image Source
Dorsal Interossei
Interossei muscles also flex the MCP joints and extend the IP joints, additionally they also serve to abduct digits 2-4 away from the midline. The dorsal interossei are innervated by the deep branch of the ulnar nerve. All of the dorsal interossei are bipennate

Image Source
Palmar Interossei
There are 3 palmar interossei flex the MCP joints and extend the IP joints and adduct digits 2,4, and 5 towards the midline. They are all unipennate, and are innervated by the deep branch of the ulnar nerve.

Image Source
Thenar Muscles
Abductor pollicus brevis
Abducts the thumb, it is also responsible for some opposition. Also supplied by the recurrent median nerve

Flexor Pollicus brevis
Flexes the thumb at the MCP joint. It is innervated by the recurrent median nerve.

Image Source
Opponens Pollicus
Allows opposition of the thumb, also supplied by the median recurrent nerve.

Image Source
Hypothenar Muscles
Opponens digiti minimi
moves 5th metacarpal towards thumb in opposition. It is innervated by the deep branch of the ulnar nerve

Image Source
Flexor digiti minimi
Flexes the proximal phalanx of 5th digit, innervated by the deep branch of ulnar nerve.

Image Source
Abductor digiti minimi
Abducts 5th digit away from midline, innervated by the deep branch of the ulnar nerve.

Image Source
Extensor Hood 13
The Extensor hood is a complex of tendons and ligaments that attaches to the phalanges. Its main function is to distribute the forces of muscle contractions to the correct locations for proper movement. The main muscles that insert on the extensor hood are the extensor digitorum, interossei, flexor digitorum profundus, and lumbricals. Extendor digiti minimi inserts on the extensor hood on the dorsal 5th digit and extensor indices attaches to the extensor hood mechanism on the dorsal 2nd digit.

Image Source
Hand Evaluation
Palpation
To feel for abnormalities in patients hands therapists can palpate. When palpating therapist should use the surface of the fingers and the hands to feel for abnormalities i.e. skeletal abnormalities, tenderness, skin deformities, skin temperature changes, and swelling.
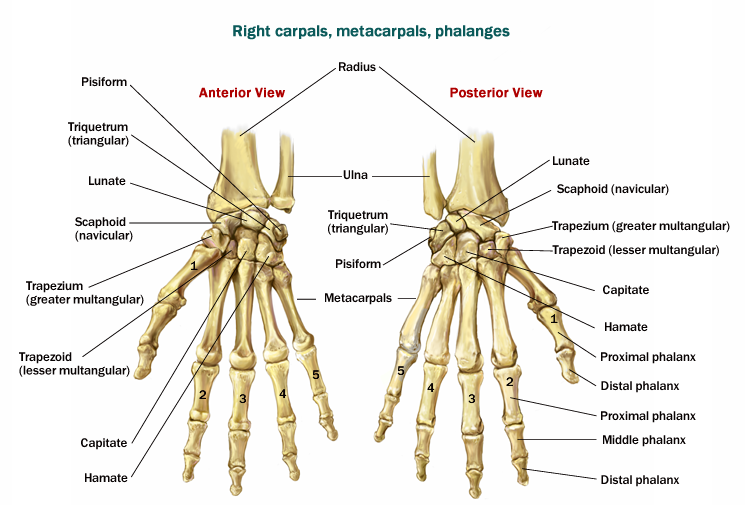
ROM 15,16
To obtain an accurate and objective measure of the amount of motion present, determine if the joint is restricted, and to detect muscle weakness in patients hands therapists measure active and passive ranges of motion (ROM). The mostly used tool for measuring ROM is the goniometer. The goniometer’s design allows the therapist to measure 0-180 degrees in the clockwise and anticlockwise direction. A minus sign is used to denote lack of extention and a positive sign denotes hyperextension. When evaluating the hand measure the following ROMs:
| ~ Motion | Testing Position | Axis | Proximal Arm | Distal Arm | Normal Range |
|---|---|---|---|---|---|
| MCP Flexion/extension | Sitting with hand off the table. Forearm and wrist in neutral | Over dorsal MCP joint | Dorsal midline of metacarpal | Dorsal midline of proximal phalanx | 900 Flexion, 300 extension |
| ~ Motion | Testing Position | Axis | Proximal Arm | Distal Arm | Normal Range |
|---|---|---|---|---|---|
| MCP Abduction/Adduction | Sitting with hand off the table, full pronation, and wrist in neutral | Over dorsal MCP joint | Dorsal midline of metacarpal | Dorsal midline of proximal phalanx | 200 Flexion, 200 extension |
| ~ Motion | Testing Position | Axis | Proximal Arm | Distal Arm | Normal Range |
|---|---|---|---|---|---|
| PIP Flexion/Extension | Sitting with hand off the table, forearm, wrist, and MCP in neutral | Over dorsal PIP joint | Dorsal midline of proximal phalanx | Dorsal midline of middle phalanx | 1000 Flexion, 00 extension |
| Motion | Testing Position | Axis | Proximal Arm | Distal Arm | Normal Range |
|---|---|---|---|---|---|
| DIP Flexion/Extension | Sitting with hand off the table, and wrist in neutral | Over dorsal DIP joint | Dorsal midline of middle phalanx | Dorsal midline of distal phalanx | 700 Flexion, 00 extension |
| Motion | Testing Position | Axis | Proximal Arm | Distal Arm | Normal Range |
|---|---|---|---|---|---|
| 1st CMC palmer flexion/extension | Sitting with hand off the table, supination, forearm and wrist in neutral | Palmar aspect of 1st CMC joint | Ventral midline radius | Ventral midline of 1st metacarpal | 300 Flexion, 100 extension |
| Motion | Testing Position | Axis | Proximal Arm | Distal Arm | Normal Range |
|---|---|---|---|---|---|
| 1st CMC palmer abduction/adduction | Sitting with ulnar border on the table, forearm and wrist in neutral | Lateral aspect of radial styloid process | Lateral midline of 2nd metacarpal | Ventral midline of 1st metacarpal | 300 Flexion, 100 extension |
| Motion | Testing Position | Axis | Proximal Arm | Distal Arm | Normal Range |
|---|---|---|---|---|---|
| 1st MCP Flexion | Sitting with ulnar border on the table, forearm and wrist in neutral | Dorsal aspect of the MCP | Dorsal midline of the metacarpal | Dorsal midline of proximal phalanx | 500 Flexion, 00 extension |
| Motion | Testing Position | Axis | Proximal Arm | Distal Arm | Normal Range |
|---|---|---|---|---|---|
| 1st IP Flexion | Sitting with ulnar border on the table, forearm and wrist in neutral | Dorsal surface of IP | Dorsal aspect of proximal phalanx | Dorsal midline of proximal phalanx | 800 Flexion, 00 extension |
Girth 16
Patients presenting with edema post trauma or surgery can be evaluated by measuring the circumference of the swollen area. When measuring, anatomic landmarks are used as reference points for the placement of the tape measure. When the edema is not be localized, making the use of tape measure highly inaccurate, the therapist can use the volumetric method. The volumetric method measures the volume of water displaced by the edematous hand. The volume displaced from the edematous hand it then compared to the contralateral side.
The picture below shows the set up for measuring edema using the volumetric method.
Volumetric Method  Image Source Image Source |
Tape measure Method |
Manual Muscle Testing9
Use the break test to measure the strength of the muscles. The break test employs the concept of placing a muscle at a point in the range were it is most challenged and manual resistance is applied. The resistance should always be in the direction of pull of the participating muscle. The examiner should instruct the patient to "hold" and not allow the examiners resistance to win. The grades to denote the different levels of strength range from 0-5. The grade are based on several factors of testing and responses by the patient. The numerical grades can be paired with words, as shown below.
| Numerical Score | Quantitative Score |
|---|---|
| 1 | Normal |
| 2 | Good |
| 3 | Fair |
| 4 | Poor |
| 5 | Trace activity |
| 0 | Zero (no activity) |
The list below shows which muscles are responsible for movement in the hand or the wrist. Weakness in the manual muscle tests can be traced to the muscles which are responsible for the movement.
- Flexor Carpi Radialis and Flexor Carpi Ulnaris (Wrist Flexion)
- Extensor Carpi Radialis Longus, Extensor Carpi Radialis Brevis, and Extensor Carpi Ulnaris (Wrist Extension)
- Lumbricales and Interossei (Finger MP Flexion)
- Flexor Digitorum Superficialis and Flexor digitorum profundus (Finger PIP and DIP Flexion)
- Extensor Digitorum, Extensor Indicis, and Extensor Digiti minimi (Finger MP Extension)
- Dorsal Interossei (Finger Abduction)
- Palmer Interossei (Finger Adduction)
- Flexor Pollicis Bravis and Flexor Pollicis Longus (Thumb MP and IP Flexion)
- Extensor Pollicis Bravis and Extensor Pollicis Longus (Thumb MP and IP Extension)
- Abductor Pollicis Bravis and Abductor Pollicis Longus (Thumb MP and IP Abduction)
- Adductor Pollicis (Thumb adduction)
- Opponens pollicis and Opponens digiti minimi ( Thumb to little finger Opposition)
Neurologial testing 12
Dermatomes
To test dermatomes use a pointed object to make contact repediatly over a particular dermatome and compare it to the same dermatome on the other side of the body. Differences in perception may indicate a problem on the side with diminished sensation.
 Image Source
Image Source
Myotomes
The examiner is to resist the subjects movements in the following positions to test for proper nerve conduction
1. Neck flexion: C1-C2
2. Neck side flexion C3 and Spinal Accessory nerve
3. Shoulder elevation C4 and Spinal Accessory nerve
4. Shoulder abduction C5
5. Elbow flexion and wrist extension C6
6. Elbow extension and wrist flexion C7
7. Thumb extension and ulnar deviation C8
8. Abduction and adduction of the fingers T1
Peripheral nerve testing
In order to do peripheral nerve testing it is necessary to test a muscle for strength that is innervated by the same nerve root as the peripheral nerve in question but that is also not supplied by the same peripheral nerve in question. If the muscle supplied by the peripheral nerve in question is weak, but another muscle supplied by a different peripheral nerve but with the same nerve root has no weakness, then the peripheral nerve in question has a problem. For sensation issues a peripheral nerve map and a dermatome map can be used to differentiate the origin of a sensory problem
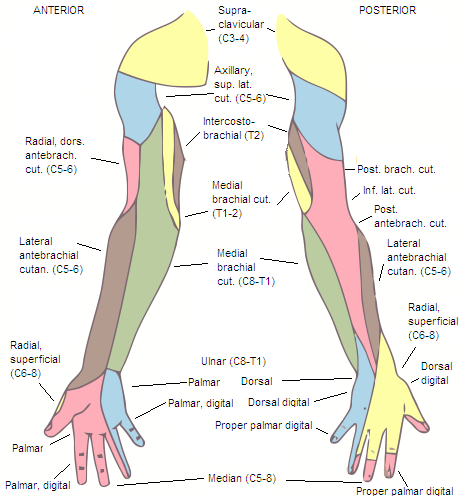
Image Source
Reflexes
Hoffmans
Detects upper motor neuron lesion. In this test the patient’s distal phalanx or fingernail is flicked on the middle or ring finger. A positive response would be a the patient exhibiting flexion in the thumb or index finger
Special Tests 12,16
Percussion Test
The patient extends his/her finger and the examiner taps the end of the finger. This test is used to look for fracture, the examiner is checking for pain.
MP Torsion or Grind test (Transverse Compression Test)
The patient extends his/her finger and the examiner stabilizes and provides compression to the distal phalanx forcing it proximally. This test also checks for fracture and the examiner looks for pain as a positive sign
Finkelstein Test
The patient makes a fist around his/her thumb. The examiner then grasps the fist and stabilizes the patient’s wrist, at the same time the fist is put into ulnar deviation. A positive sign is pain at the Abductor pollicus longus and the Extensor pollicis brevis. This test is used to diagnose tenosynovitis in Abductor pollicus longus and the Extensor pollicis brevis.
Phalen Test
The patient flexes both wrists to end range and the examiner applies a compressive force pushing the hands together for one minute. A positive sign for this test is numbness and tingling in areas where the median nerves innervates. This test is used to detect carpal tunnel syndrome.
Tinels Test
The patient exposes the volar aspect of his/her wrist and the examiner taps the wrist at the carpal tunnel. A positive test is numbness, tingling, pins and needles, or pain in the sensory area in which the median nerve innervates. This test can indicate carpal tunnel syndrome.
Brunnel littler Test
The examiner first extends the wrist to lengthen the extrinsic wrist extensors and keep them from interfering with the test. Then the examiner flexes the patient’s proximal IP joint and looks at available flexion ROM with the MP extended. The examiner then flexes the MP joint and looks at available flexion ROM in this position in the proximal IP joint. A positive test is indicated if in MP flexion the proximal IP joint cannot also flex as this indicates capsule tightness. A positive test for intrinsic muscle tightness is found if in the extended MP position the proximal IP joint cannot go through its full range of motion.
Murphy’s Sign
The patient makes a fist and the examiner checks for the third metacarpal location. If the 3rd metacarpal is at the same level as the 2nd and 4th metacarpals that is a positive sign. A positive sign indicates a dislocated lunate.
Valgus Stress Test (Ulnar/Radial stress test)
In this test the examiner stabilizes a distal phalanx while providing a varus and valgus force on the proximal phalanx. A positive sign would be excessive gapping or pain. A positive sign indicates a collateral ligament sprain or tear.
Fromet’s Sign
The patient holds a piece of paper between the thumb and the index finger and the examiner tries to pull it away. A positive sign would be flexion in the first IP joint and would indicate Adductor pollicus paralysis because of ulnar nerve problems. If MCP extension occurs with first IP joint flexion this would indicate more extensive damage to the ulnar nerve, this is known as Jeanne’s sign.
Long Finger Flexion test
The examiner stabilizes the MCP and PIP, and has the patient then flex the DIP. A positive sign is loss of flexion at the DIP. This indicates FDP rupture or damaging to the nerves innervating FDP. A variation of the test is to stabilize only the MCP and have the patient try and flex the PIP and DIP, if the patient is not able to flex either then both the Flexor digitorum profundus and superficialis are involved.
AIN Test
The patient is asked to make an “OK” sign with his/her hands by pinching the thumb and index fingers together. If the patient is unable to do so and instead produces a square shape instead with his/her fingers this indicates the loss of FPL and FDP and thus the loss of the AIN.
PIN Test
The examiner asks the patient to extend the hand at the wrist. If the patient also radially deviates this is a positive sign. This is because ECU is supplied by the PIN and so it can not counter ECRL and Brachioradialis supplied by the radial nerve.
Wartenburgs Sign
The patient has his/her hand pronated on a flat surface and extends the digits. Then the patient abducts and adducts the hand in this position. A positive sign is an inability to adduct the 5th digit, this occurs because of the unopposed action of EDM in certain ulnar nerve pathologies.
Functional tests
Hand grip test16,9
Therapist uses a dynamometer to asses the patients grip strength. Patient should be positioned in a shoulder adducted, elbow at 900 flexion, and wrist and forearm in neutral. The first position of the dynamometer is the least advantages because it mainlyrelies on the intrinsic muscles and the fifth position is most advantages because both the intrinsic and extrinsic musculature contrubute to the contraction.
Other Grip Tests
Give the patient different object to hold and observe the strength of the grip. The video below demonstrates the different grips.
Typical Pathologies
Guyons Canal Syndrome
The Ulnar nerve becomes entrapped between the pisiform and hamate bones and the Pisohamate ligament. This condition is also known as handlebar palsy as it can often be seen in bikers due to weight bearing on their carpal bones. It can have many causes including hamate fracture, ganglion cysts, ulnar artery compromise, and simply putting too much pressure on the area.
Guyon's canal Structures8,1
| Floor | ranverse carpal ligament, pisohamate ligament, pisometacarpal ligament, opponens digiti minimi |
|---|---|
| Roof | Volar carpal ligament |
| Ulnar wall | Pisiform and abductor digiti mini |
| Radial wall | Hook of Hamate |
Guyon's Canal Zones8,1
| Zone 1 | Proximal to bifurcation of nerve | mixed motor/sensory symptoms |
|---|---|---|
| Zone 2 | Surround deep motor branch. Ganglia and hook-of-hamate pathology are common causes | motor symptoms only |
| Zone 3 | Surrounds superficial sensory branch. Ulnar artery thombosis is common cause | sensory symptoms only |
Carpal Tunnel Syndrome6,2
In true carpal tunnel syndrome there should only be sensation problems in the first three digits and half of the fourth digit. Sensation problems can include numbness and tingling, pins and needles, and pain. Motor functioning can also become disrupted leading to lack of coordination and muscle weakness. Carpal tunnel syndrome is caused by compression on the median nerve when it runs through the carpal tunnel. Compression occurs when the Median nerve is forced against the flexor retinaculum by inflamed structures in the carpal tunnel.
Ulnar Claw
When there is an ulnar nerve lesion, the 4rd and 5th digit are extended at mcp and flexed at ip joints because the interossei and 3rd and 4th lumbricals are not active. The hypothenar muscles are also knocked out, so flexion, adduction and opposition in the little finger are also nonexistent. Of the thenar muscles adductor pollicus is the only one to be effected.
Popes hand
This configuration is only appearent when making a fist. Here lumbricals 1 and 2 as well as the lateral half of the FDP are not functioning due to a high median nerve lesion. When making a fist only digits 4 and 5 move into flexion. There will also be paralysis of the thenar muscles and thus no opposition and abduction of the thumb.
Bibliography
1. Carmeli E, Hagar Patish, Coleman R. The aging hand. The Journals of Gerontology. 2003;58A(2):146-52.
2. Claude Pierre-Jerome, Robert D Smitson Jr, Raj K Shah, Valeria Moncayo, Michael Abdelnoor, Michael R Terk. MRI of the median nerve and median artery in the carpal tunnel: Prevalence of their anatomical variations and clinical significance. Surgical and Radiologic Anatomy. 2010;32(3):315-322.
3. Goldner JL, MD, Rozmaryn LM, MD. Overuse tendinitis. Orthopedics. 1999;22(3):288-289.
4. P. Chaynes, J. Bécue, P. Vaysse, M. Laude. Relationships of the palmar cutaneous branch of the median nerve: A morphometric study. Surgical and Radiologic Anatomy. 2004;26(4):275-280.
5. Schachar NS. Musculoskeletal images. ganglion cyst of guyon's canal causing ulnar nerve compression. Canadian Journal of Surgery. 2001;44(5):331-2.
6. Schoen DC. Upper extremity nerve entrapments. Orthopaedic Nursing. 2002;21(2):15-31; quiz 31-2.
7. Worrell M. Dupuytren's disease. Orthopedics (Online). 2012;35(1):52-60.
8. Moore, Derek. Ulnar Tunnel Syndrome. Orthobullets.www.orthobullets.com/hand/6022/Ulnar-tunnel-syndrome.
9. Kendall, F. Muscles Testing and Function with Posture and Pain. 5th Ed. Baltimore, MD: Lippincott Williams & Wilkins;2005.
10. Magee, D. Orthopedic physical assessment. 5th Ed. S. Louis, MO: Saunders;2008.
11. Banks, K. Maitland's Clinical Companion. Edinburgh, U.K.: Churchill Livingstone Elsevier;2010.
12. Gulick, D. Ortho Notes Clinical Examination Pocket Guide. 2nd Ed. Philadelphia, PA: F.A. Davis Company; 2009.
13. Newport ML, Tucker RL. New perspectives on extensor tendon repair and implications for rehabilitation. Journal of Hand Therapy. 2005;18(2):175-81.
14. Examination of the hand. Orthofracs: Orthopaedic surgey resource for doctors. 2012. Available at: http://www.orthofracs.com/clinical/examination/hand/special-tests.html.Accessed Nov 26, 2012
15.Bandy W,Reese N.Joint Range of Motion and Muscle Length Testing.St Louis, MS:Saunders Elsevier;2010:473.
16. Bear-Lehman J, Abreu BC. Evaluating the hand: Issues in reliability and validity. Physical Therapy. 1989;69(12):1025-1033.














