by Katie Blackwell
Description
Cluster headaches are an excruciatingly painful form of headache, so much so that they are also termed “suicide headaches.”1 They are classified by relatively short but severe episodes of pain with autonomic dysfunction. The pain and dysfunction occurs ipsilaterally and pain tends to be centralized to the eye and the orbital area. Cluster headaches have bouts of attacks and then remission periods. The bouts tend to be at the same time(s) of year for every occurrence and may last for weeks or months at a time. Attacks begin and end rather suddenly and take place once every other day or up to 8 times a day, often at night.1,2,3,4,5,6 In periods of remission no headaches are experienced. Depending on the length of this remission period, cluster headaches may be considered to be episodic or chronic.1-3 The cause of cluster headaches is still unknown despite several theories. These types of headaches are rare and hard to diagnose and therefore often mistaken for other types of headaches. Further explanation, classification and treatments are posed below.
Etiology

The cause of cluster headaches is unknown. Cluster headaches occur in a circannual or circadian cycle, with peaks sometimes following the solstices. Attacks also tend to take place at the same time of day during each bout.1-3 Due to these factors specific to cluster headaches, researchers have had some success in describing a hypothalamus mechanism as this is the area that controls the biological clock. Another possible cause is based on a neurovascular theory with vasoconstriction and dilation of blood vessels affecting the trigeminal nerve. However, this thought is not clear if it is a symptom or a cause. Other causes include levels of substances in the body, such as histamine, that might be linked to the autonomic dysfunction or a genetic link.1-2
Classification
Cluster headaches are classified as a trigeminal autonomic cephalagia (TAC) which are a primary headache disorder. Primary headache disorders mean that there is no underlying cause, such as a lesion or tumor.1-6 TACs consist of pain unilaterally and in the trigeminal nerve distribution with a form of autonomic dysfunction. There are 3 types of TACs, cluster headaches, paroxysmal hemicrania and SUNCT (short unilateral neuralgiform headache with conjunctival injection and tearing), with cluster headaches being the most common.1-5
Incidence/ Prevalence
Cluster headaches are not frequently diagnosed. It has been estimated that they affect .1% of the population.1,3 In one headache care clinic, cluster headaches were diagnosed less than 3% of the time.2 Men are more often affected with a range of 2-7:1 ratio of males to females.1-3,6 The large range is due to the increased recognition of cluster headaches and TACs, especially in women. Often, due to the low incidence of this type of headache, there is a median delay of 3 years before diagnosis. These types of headaches in children are rare.2 Peak incidence has been observed in the 3rd 2 decade through the 5th decade.1 Often, symptoms decrease or cease altogether after 70 years of age.2
Pain
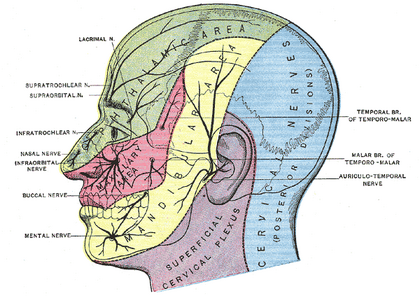
Cluster headache pain is described as ipsilateral and generally in the first trigeminal branch distribution. However, pain can also be experienced as radiating to the temporal, occipital, and cervical regions as well as the teeth.1-3,5 It has been estimated that 60% of patients have pain on the right side,1 yet a small percentage of patients have headaches that may switch sides during or in subsequent attacks.1-3 Lying still does not help these patients and may actually make the pain worse.2
Autonomic Dysfunction
Signs of autonomic dysfunction are also present during the cluster headache attacks. Usually the symptoms are on the same side as the pain. These symptoms may include tearing of the eye, swelling of the eyelid, a runny or stuffy nose, sweating of the face, and redness of the face or eye. These factors may be subtle or very pronounced.1-6
Clinical Presentation
Patients with cluster headaches are in obvious, excruciating, single-sided pain. Some patients may describe the pain as someone sticking a hot poker in their eye and possibly for female patients, worse than childbirth.1-3,6 These patients are agitated and tend to sit and rock back and forth, sometimes even beating their head.1-2 Lying down and being quiet does not help. Pain comes on suddenly, usually with no warning that it is about to. Along with the pain is the autonomic dysfunction such as redness, nose congestion or tearing.1-6 The headaches last anywhere from 15 to 180 minutes1-3 and they often come on after the patient goes to sleep, during the first rapid-eye-movement (REM) cycle.1 Pain also ceases suddenly when the attack is done. These attacks occur anywhere from once every other day to 8 times a day.1-3
Diagnostic Methods
The only way to diagnose a cluster headache is through the patient's history unless an attack is witnessed. The criteria is decided and spelled out by the International Classification of Headaches.1-3,5 The second edition of this describes the factors of a cluster headache as well as if it is episodic or chronic.
International Classification of Headache Diseases II diagnostic criteria for cluster headaches2
- At least 5 attacks fulfilling the following
- Severe or very severe unilateral orbital, supraorbital and/or temporal pain lasting 15 to 180 minutes if untreated
- Attacks have a frequency from 1 every other day to 8 per day
- Not attributed to another disorder
- Headache is accompanied by at least one of the following:
- Ipsilateral conjunctival injection and/or lacrimation
- Ipsilateral nasal congestion and/or rhinorrhea
- Ipsilateral eyelid edema
- Ipsilateral forehead and facial sweating
- Ipsilateral miosis and/or ptosis
- A sense of restlessness or agitation
The criteria for episodic or chronic first has to fulfill everything listed above. Then episodic is described as at least two cluster periods lasting from 7 to 365 days and separated by pain free remissions of more than one month. Chronic cluster headaches are attacks that recur for greater than one year without remission periods or with remission periods lasting less than one month.1-3
Neuroimaging typically does not show any significant findings for cluster headache patients. However, there have been studies that show cluster headaches caused by lesions in the brain, so neuroimaging is recommended for all cluster headache and TAC patients.4
Potential Etiologies
Due to the low incidence of cluster headaches there is usually a long list for the differential diagnosis. The list includes, but it not limited to:1-6
- other types of headaches, especially migraines or hypnic heaches
- other TACs
- trigeminal neuralgias due to the pattern of pain
- orbital myositis, but these typically have a longer duration
- a secondary cause such as a lesion on the pituitary or another location
Conservative Treatment
Normal analgesic medications do not work for a cluster headache. The medications and treatments that do have the greatest effect are either abortive, or significantly decrease or end the attack, or prophylactic, to decrease the number of attacks. Some of the treatments are described in depth on the American Headache Society- Treatment of Cluster Headaches page under Web-Based Resources.
- Abortive medications1-3,6
- Oxygen- 100% oxygen at a flow rate of 10-15 L/min
- Triptans- a class of drugs that includes sumatriptan (Imitrex)
- these drugs need to be administered via injection or nasal spray as oral medications of this form are not quick enough
- Prophylactic medications1-3,6
- Triptans-oral, daily
- Steriods- either as oral or injection
- Lithium
- Methysergide
- Verapamil
- Ergotamine
- As well as various others
Therapeutic Modalities
When completing a PubMed search for pertinent modalities to assist in cluster headache treatment, very little was presented. A search was performed for any full text, English language articles using the key words “cluster headache” and “physical therapy,” “therapeutic modality,” “modality,” “treatment,” “therapeutic exercise,” “ needling” and “trigger point.”
Most of the evidence being returned was about the medical management. This included the pharmacological approach, including the use of oxygen.7 Although physical therapists utilize this tool with patients, it is considered a drug due to the need of a prescription for it. Another popular result from the search was the use of implanted occipital nerve stimulators or hypothalamic deep brain stimulation. These are both surgical approaches to electrical stimulation. Implantable electrode placement at the posterior aspect of C1-3 stimulates the occipital nerve thereby affecting the trigeminocervical complex.8 The speculation that the trigeminal nerve is one of the contributing factors of a cluster headache is what has led to this method for these types of headaches.8 However, it seems that this method is more effective for migraine and other headaches.8 Deep brain stimulation has been done due to the activation of the hypothalamus during cluster headaches.9 This type of stimulation has also shown promising effects for cluster headache patients,9 however both surgeries have serious risks associated with them.8,9
While the medical management of cluster headaches has supporting literature, physical therapy tools are only speculations mentioned in passing. It has been suggested to include exercises that help neck movement restrictions and stiffness if present.10 A preliminary research report found evidence that patients with cluster headaches have myofascial trigger points, similar to other primary headache diagnoses.11 The surprising presence of trigger points allowed for needling of the sites with some success.11 Other than these limited interventions, the research of modalitites and PT for cluster headache management is not well established.
Surgery
Surgical interventions are a last resort for cluster headache patients if medications provide no relief. They are not often done, but the surgeries that may be considered are:1-3
- An occipital nerve block due to its relation with the trigeminal nerve
- Electrode on occipital nerve to decrease firing
- Trigeminal nerve rhizotomy of the first sensory branch
- Hypothalamic deep brain stimulation
What the Physical Therapist Should Know
It is most likely that patients with these types of headaches would seek other medical treatment before a physical therapist would see them. However, a PT should still be aware of these types of headaches and what makes them unique. A PT should know what could potentially trigger a cluster headache. There are only a few and they only perpetuate an attack during a cluster bout. These triggers are alcohol, nitroglycerin, strong odors, smoking and taking naps.1-3 In general, a PT should know where to direct the patient for more information if needed. Headache diaries are very useful to observe patterns of headaches and could be suggested by the PT if the patient does not already do so.
Additional Web Based Resources
Cluster Headache Fact Sheet from City of London Migraine Clinic
City of London Migraine Clinic Audio and Video
American Headache Society- Treatment of Cluster Headaches
American Headache Society- Headache Diaries
Mayo Clinic- Cluster Headache
NIH Medline Plus- Cluster Headaches










